How to Clean Your Eyelids
Experiencing eyelid inflammation or frequent styes? Kyle teaches and demonstrates a variety of great techniques for eyelid and lash hygiene.
Cataract Surgery Post-Op Instructions
Please enjoy these helpful tips and instructions for caring for your or a loved one’s eyes after cataract surgery.
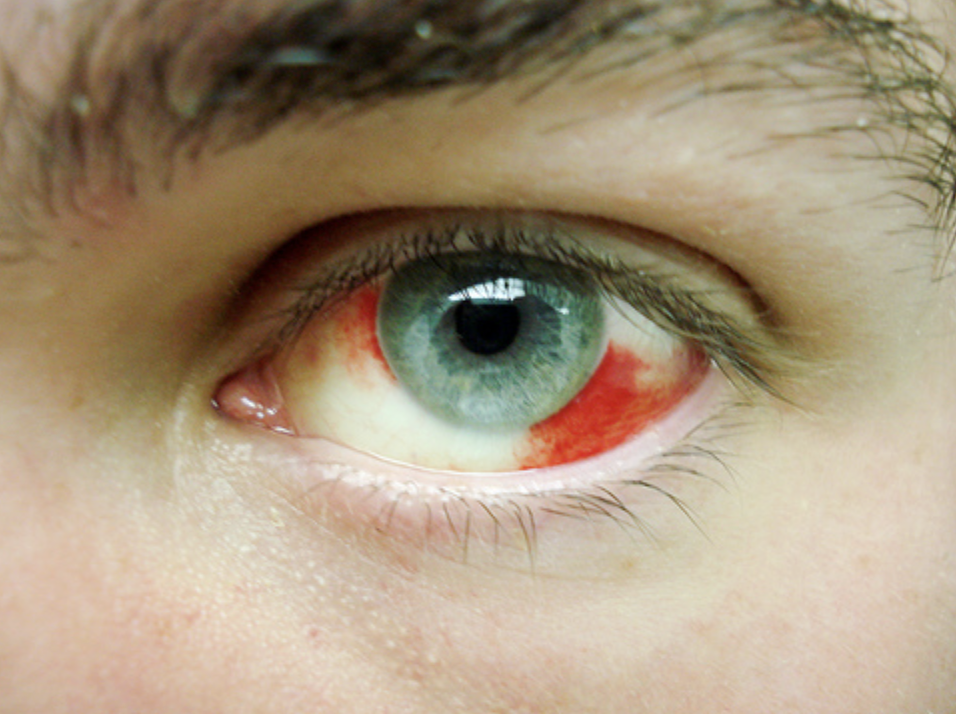
Red Eye: What is a Subconjunctival Hemorrhage?
Have you ever woken up with a bloody red spot in your eye? You might have what ophthalmologists call a subconjunctival hemorrhage. Want to know more about what to do? Read on!
Have you ever woken up with a bloody red spot in your eye? You might have what ophthalmologists call a subconjunctival hemorrhage. Want to know more about what to do? Read on!
A subconjunctival hemorrhage happens when blood vessels in your eye’s conjunctiva break or leak. The conjunctiva is the clear tissue covering the white part of your eye. When they break, the blood can leak between the conjunctiva and sclera, causing a red spot to appear in your eye. These blood spots often look much scarier than reality, and subconjunctival hemorrhages usually are harmless and heal on their own.
Symptoms:
A subconjunctival hemorrhage usually appears as a bright red or dark patch on the white of the eye, and thankfully, that’s typically the only symptom. While it may look alarming, it’s generally painless. Some people may feel a mild scratchy sensation, and you might also notice the blood shifting position as it resolves.
Causes:
This condition often results from a sudden increase in pressure within the body, such as from heavy lifting, intense coughing or sneezing, or even straining during a bowel movement. These actions can cause tiny blood vessels in the eye (capillaries) to break.
In other cases, it can occur due to trauma to the eye or excessive rubbing. While less common, certain medical conditions like high blood pressure, diabetes, or blood-clotting disorders may increase the risk. Medications like aspirin or blood thinners may make you more susceptible to subconjunctival hemorrhage..
Treatment:
The good news is that no treatment is usually necessary. We recommend an examination with your eye doctor to confirm there is no other damage or underlying disease in the eye that requires attention. The blood will naturally be reabsorbed by your body, often clearing up within a few days to a few of weeks, depending on the size. If the eye feels irritated, over-the-counter artificial tears can help soothe discomfort. If you notice this happening repeatedly, your healthcare provider might recommend a blood test to check for underlying issues.
All in all, subconjunctival hemorrhages are often less scary than perceived, and with a bit of time, your body does all the work to heal it!
How to Use Hot Compresses
Hot compresses are a simple, effective, at-home treatment for a variety of common eye conditions. Whether you are dealing with dry eye, meibomian gland dysfunction (MGD), or stubborn styes and chalazia, applying consistent heat can help relieve symptoms and promote healing.
Hot compresses are a simple, effective, at-home treatment for a variety of common eye conditions. Whether you are dealing with dry eye, meibomian gland dysfunction (MGD), or stubborn styes and chalazia, applying consistent heat can help relieve symptoms and promote healing.
You may be tempted to reach for a warm washcloth, but unfortunately, it cools off too quickly to be effective. Instead, here are a few tried-and-true methods that provide longer-lasting, consistent warmth:
Rice in a Sock - One of the easiest DIY options!
Place uncooked rice in a clean sock and tie it off
Microwave for about 30 seconds (adjust time as needed)
Microwaveable Eye Mask - For a convenient, targeted option, consider a microwaveable eye mask.
We recommend the Oasis Eye Mask, which is available in our office
Microwave the mask for 30-40 seconds.
Strap it on, close your eyes, and relax for 10-15 minutes.
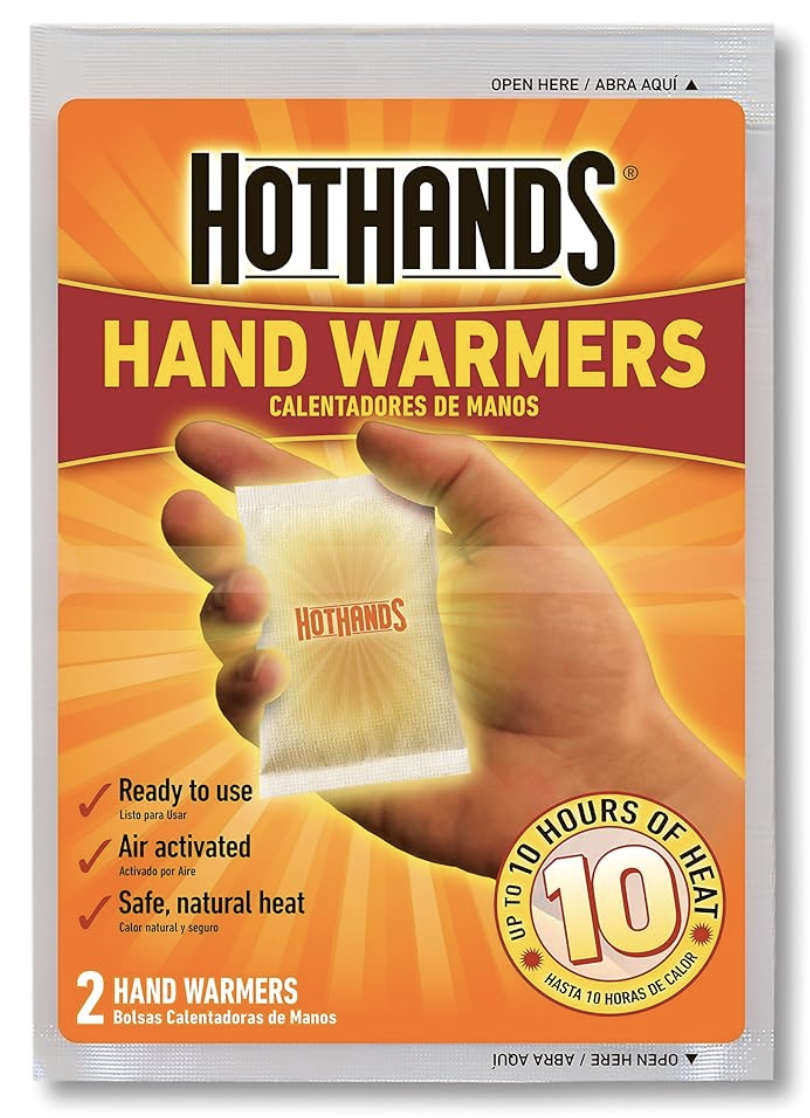
Hand Warmers (“HotHands”) - This creative tip came from Dr. Khine while she was on a ski trip!
Hand warmers stay hot for up to 10 hours, making them an excellent option for on-the-go use.
Simply activate the warmer and place it inside a soft eye patch.
This hands-free method allows you to keep the compress on throughout the day while doing other tasks, especially helpful for treating styes.
Tips for the Best Results
Always check the temperature before applying any compress to avoid burns
Aim for 10 minutes per session, multiple times daily if needed.
Keep your eyes closed while using the compress.
If symptoms persist or worsen, consult your eye care provider.
Consistent use of a hot compress can make a big difference in managing eye conditions. Feel free to ask any of our staff at Focus Eye Center if you have questions or need recommendations! Call to schedule an appointment!
Cómo Usar Compresas Calientes
Las compresas calientes son un tratamiento casero simple y eficaz para una variedad de afecciones oculares comunes. Ya sea que estés lidiando con ojo seco, disfunción de las glándulas de Meibomio (DGM), orzuelos y chalaziones persistentes, aplicar calor de manera constante puede ayudar a aliviar los síntomas y promover la curación.
Las compresas calientes son un tratamiento casero simple y eficaz para una variedad de afecciones oculares comunes. Ya sea que estés lidiando con ojo seco, disfunción de las glándulas de Meibomio (DGM), orzuelos y chalaziones persistentes, aplicar calor de manera constante puede ayudar a aliviar los síntomas y promover la curación.
Puede que sientas la tentación de usar un paño tibio, pero desafortunadamente, se enfría demasiado rápido para ser eficaz. En su lugar, aquí te presentamos algunos métodos comprobados que proporcionan calor constante y de mayor duración:
Arroz en un calcetín – ¡Una de las opciones caseras más fáciles!
Coloca arroz crudo en un calcetín limpio y átalo bien.
Caliéntalo en el microondas durante unos 30 segundos (ajusta el tiempo según sea necesario)
Mascarilla ocular para microondas – Una opción práctica y específica
Considera usar una mascarilla ocular para microondas.
Recomendamos la mascarilla Oasis, disponible en nuestra clínica.
Caliéntala en el microondas durante 30-40 segundos.
Colócatela, cierra los ojos y relájate durante 10-15 minutos.
Calientamanos (“HotHands”)
¡Este ingenioso consejo vino de la Dra. Khine mientras estaba en un viaje de esquí!
Los calientamanos se mantienen calientes por hasta 10 horas, lo que los convierte en una excelente opción para usar mientras estás en movimiento.
Simplemente activa el calientamanos y colócalo dentro de un parche ocular suave.
Este método manos libres te permite mantener la compresa puesta durante todo el día mientras realizas otras actividades, lo cual es especialmente útil para tratar orzuelos.
Consejos para obtener los mejores resultados
Siempre revise la temperatura antes de aplicar cualquier compresa para evitar quemaduras.
Apunte a sesiones de 10 minutos, varias veces al día si es necesario.
Mantenga los ojos cerrados mientras usa la compresa.
Si los síntomas persisten o empeoran, consulte a su proveedor de atención ocular.
El uso constante de una compresa caliente puede marcar una gran diferencia en el manejo de afecciones oculares.
¡No dude en preguntar a cualquiera de nuestro personal en Focus Eye Center si tiene preguntas o necesita recomendaciones! ¡Llame para programar una cita!
What is Clear Lens Extraction?
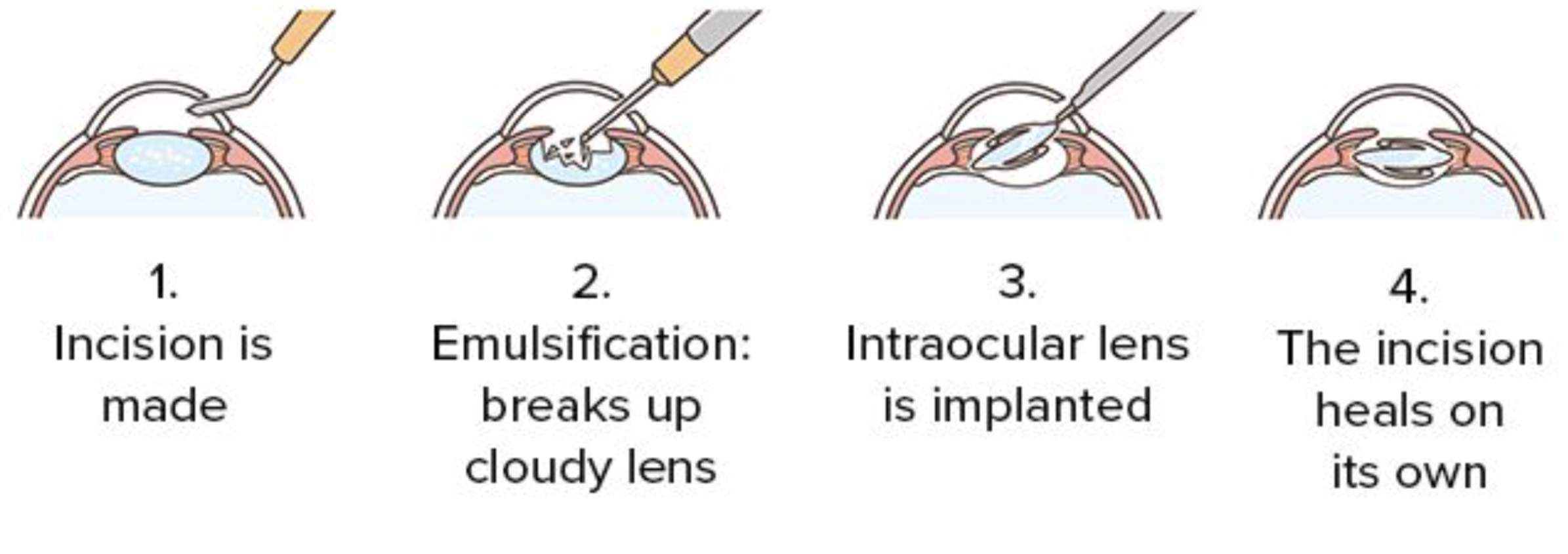
CLE is a procedure similar to cataract surgery, in which an ophthalmologist will remove the natural lens of your eye and replace it with an artificial lens. This lens implant corrects your prescription inside your eye, eliminating your dependence on glasses or contacts.
While glasses and contact lenses are often sufficient for vision correction, many wish to be “glasses-free.” There are various types of vision correction surgeries. The most common are LASIK and photorefractive keratectomy (PRK), which use different laser techniques to change the shape of your cornea, and thus change your glasses prescription. However, not everyone is a good candidate for LASIK or PRK, and once patients are over 40 years old, they still require reading glasses. A great alternative is “Clear Lens Extraction” (CLE), also known as “Clear Lens Exchange”. Keep on reading to find out more about CLE!
What is CLE?
CLE is a procedure similar to cataract surgery, in which an ophthalmologist will remove the natural lens of your eye and replace it with an artificial lens. This lens implant corrects your prescription inside your eye, eliminating your dependence on glasses or contacts.
The natural lens inside the eye becomes cloudy over time, forming a cataract, which is removed during cataract surgery and replaced with a lens implant. Clear Lens Extraction is the same procedure, but is performed before the patient develops a foggy cataract. Therefore, patients who undergo this procedure do not need to have cataract surgery again in the future, and they do not need to wait until a cataract forms to enjoy the benefits of modern lens implant technology.
Lens Options
The artificial lens can correct issues with distance vision (myopia or hyperopia) and/or near vision (presbyopia). Due to advancements in technology, there are different lens options available:
Monofocal Lenses:
These lenses correct for only one distance – either far or near – and much like LASIK, glasses are required for other distances. Historically, people who used contact lenses to correct one eye for distance vision and one eye for near vision could have the same prescriptions built into the eye with monofocal lens implants. This “monovision” strategy is less commonly used today given advances in lens technology.
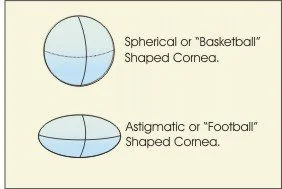
Astigmatism-Correcting Lenses:
These lenses are called toric lenses, and they can correct astigmatism on the cornea (the clear front window of the eye) and distance vision. Most people will still need reading glasses.
Multifocal and Extended-Depth-of-Focus Lenses:
Multifocal and “extended-depth-of-focus” implants correct vision simultaneously at far, intermediate, and near. Patients undergoing clear lens extraction will typically choose these lenses to obtain the full benefit of the CLE surgery. With these implants, patients can see into the distance, drive, use the computer, and read a phone, tablet, or book, all without glasses. However, not everyone is a candidate for multifocal lenses, and your ophthalmologist must rule out eye disease such as macular degeneration and glaucoma.
The Process
During the evaluation appointment, a patient will have a full exam done by an ophthalmologist to determine whether the patient is a good candidate for CLE. Precise measurements of the eye are taken, and the ophthalmologist will go over the different types of lens options and determine the best fit for the patient.
Surgery is performed in the operating room and takes about ten minutes. Patients will receive numbing medication and IV anesthesia. The ophthalmologist will then make tiny laparoscopic incisions to remove the natural lens and replace it with the artificial lens. The eyes are treated on different days, typically a week or two apart. Patients take post-op drops to help with the healing process and return for post-op visits a day after surgery, a week after surgery, and a month after surgery. Since CLE is a permanent process, patients can expect their prescription to remain stable, and they will not need cataract surgery later in life.
Ultimately, CLE is a great option for those who wish to live free of glasses and contacts. LASIK and PRK laser surgeries leave patients over 40 years of age dependent on reading glasses. Only clear lens extraction can correct both eyes for the full range of vision from far to near. Call us to schedule a consultation, and take a step forward to having CLEar vision!
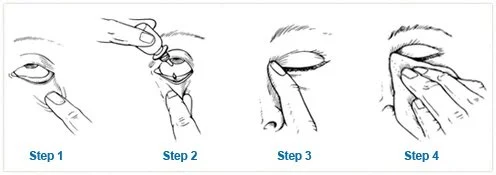
How To Use Your Eye Drops
Using eye drops or eye ointment, especially for those who are unfamiliar with touching their eyes, can be difficult and frustrating. However, with a couple of tips, tricks, and practice, anyone can learn how to put eye drops in their eyes with ease. Want to learn how to put eye drops in?
Using eye drops or eye ointment, especially for those who are unfamiliar with touching their eyes, can be difficult and frustrating. However, with a couple of tips, tricks, and practice, anyone can learn how to put eye drops in their eyes with ease. Want to learn how to put eye drops in? Refer to the tips below!
Use eye drops as follows:
Step 1: Bend your head back, and look up toward your eyebrows. With one finger, gently pull the lower lid down to form a small pocket.
Step 2: Drop the medicine into the pocket. (For ointment, squeeze a grain of rice sized amount into the pocket.) Do not touch the dropper against the eyelid or anything else.
Step 3: Close your eyes for one minute to allow your eye to absorb the medicine. Try not to blink.
While your eyes are closed, gently press your finger against the area between the inner corner of your eye and your nose. This blocks the tear drainage duct and prevents the drop from flowing into the nose and back of the throat. (Do not press on the eyeball.)
Step 4: Wipe any excess liquid that may have collected near the eye. If you are using more than one kind of eye drop, wait at least five minutes before using another eye drop. This allows the first drop to fully absorb before washing it out with the next medication. Remember, if using ointment, it can blur your vision for up to thirty minutes, so please plan accordingly.
Lifestyle Choices You Should Incorporate in Your Glaucoma Management
While lifestyle changes alone are not sufficient, patients can better control their glaucoma with these tips!
What is Glaucoma?
Glaucoma is an eye disease where high eye pressure damages the optic nerve. The eye’s drainage system can become defective and prevent fluid from properly escaping the eye. The optic nerve is like an electric cable that is responsible for transmitting signals to the brain. At first, glaucoma can cause peripheral vision loss. If the patient does not treat their glaucoma, the optic nerve becomes further damaged, which can lead to blindness. Progressive neuron loss in glaucoma is irreversible, so it is important to abide by the recommendations the doctor provides, such as using pressure-lowering drops, receiving laser treatment, or for severe cases, surgery. While there is still much to learn about glaucoma, there are ongoing studies on the effects of lifestyle choices on glaucoma. Dr. Valentina Lozano, a glaucoma specialist, and Dr. Nancy Lin, a nutritionist, divide these healthy habits into categories: physical, nutritional, environmental, mental, emotional, and spiritual. Want to know more? Keep on reading!
Physical
Three main recommendations are keeping the head upright (above your heart), avoiding sustained Valsalva maneuvers, and integrating aerobic exercise into daily life. Eye pressure can fluctuate throughout the day, yet it usually increases at night when the body is laying down. Therefore, it is recommended that patients with advanced glaucoma sleep with their heads elevated with extra pillows or with the head of the bed raised.
Additionally, patients should avoid exercises where their head is turned upside down such as downward dog yoga poses and headstands. Recently, there was research done on a patient who did headstands regularly, and there was a noticeable increase in eye pressure (15 mmHg to 33 mmHg) from when he was upright to when he was in a headstand.
A Valsalva maneuver is a forceful exhalation against a closed airway. For example, plugging one’s nose and breathing out would be considered a Valsalva maneuver. These Valsalva maneuvers often occur when lifting heavy weights, playing wind instruments, or straining to defecate, which patients with advanced glaucoma should try to avoid. Lastly, aerobic exercise can help maintain eye health and overall health. Cardio such as running, hiking, and even pickleball are great options.
Nutritional
While nutrition affects a number of conditions, there are certain foods patients should consume and avoid in managing their glaucoma. Foods containing flavonoids help slow down the progression of glaucoma by increasing blood flow to the optic nerve. Flavonoids are found in red and purple fruits and vegetables, legumes, lentils, chickpeas, caffeinated teas, and dark chocolate. Foods containing nitric oxide also help regulate eye pressure by increasing drainage outflow. Nitric oxide can be found in dark, leafy green vegetables, celery, beets, citrus, eggplant, and dark chocolate. Lastly, it is recommended to consume foods containing Omega-3, specifically the docosahexaenoic and eicosapentaenoic acids. These are found in walnuts, and seafood such as salmon, tuna, sardines, and sea algae.
While many foods are helpful for glaucoma, there are also some to avoid. Foods high in saturated fats, trans-saturated fats, and complex carbohydrates can decrease blood flow. Patients with glaucoma should monitor their intake of red meat, processed meats, dairy products, fried foods, potatoes, bread, rice, and pasta. Coffee can also increase eye pressure for short periods of time. Though one to two cups are all right to consume, patients with advanced glaucoma should limit their caffeine intake.
Environmental
The two main environmental factors that can affect glaucoma are smoking and long-term lead exposure. Nicotine in cigarettes, vapes, and chewing tobacco can increase eye pressure. Smoking can also affect patients’ dry eye symptoms. Many glaucoma patients already have dry eye as a side effect of pressure lowering drops, so smoking can further aggravate their dry eye. While studies have shown that marijuana can lower eye pressure, the effect only lasts for three to four hours, and CBD actually increases eye pressure. Ophthalmologists recommend that patients avoid using marijuana on the day of their appointment to avoid any interference with their eye pressure measurements.
Mental, Emotional, and Spiritual
While there is not much research done on the effects of stress on glaucoma, it has been shown that stress and anxiety can increase a patient’s heart rate and eye pressure, potentially mediated by the stress hormone cortisol. Yoga, breathing, and meditation are recommended to increase blood flow and decrease eye pressure. Any spiritual practice a patient wishes to adopt may help manage his or her glaucoma, by lowering stress levels and thereby lowering eye pressure.
Ultimately, various lifestyle practices can help glaucoma patients, yet the best way to treat glaucoma is to follow the doctor’s instructions. Lifestyle changes alone do not lower a patient’s eye pressure enough to control glaucoma. Since glaucoma is usually painless, irreversible, and initially asymptomatic, it is important for patients to establish a good relationship with their doctor to find the treatment most suitable to them.
References:
Boyd K. What is Glaucoma? Symptoms, Causes, Diagnosis, Treatment. American Academy of Ophthalmology. December 2023. Available at: https://www.aao.org/eye-health/diseases/what-is-glaucoma. Accessed March 18, 2024
Lozano V MD. Healthy Habits For Glaucoma Patients. Glaucoma Today. September/October 2023. Available at: https://glaucomatoday.com/articles/2023-sept-oct/healthy-habits-for-glaucoma-patients?c4src=se arch:feed. Accessed March 18, 2024
Why you should think twice about getting eyelash extensions
Are you thinking about getting lash extensions? Read this article before considering putting your eyes at risk.
Are you thinking about getting lash extensions? Read this article before considering putting your eyes at risk.
Eyelash Extensions Overview
There are different types of eyelash extensions: temporary, usually applied at home, and semi-permanent, usually applied in a salon. Temporary false lashes are applied with lash glue which is made of adhesive components, surfactants, and ammonium hydroxide. Some adhesives contain glycol ethers which are found in other cosmetics, pharmaceuticals, cleaners and other home products. Lash adhesive is typically not harmful unless swallowed or ingested, which is indicated on the label packaging. On the other hand, semi-permanent lash extensions are applied on each strand of one’s natural eyelashes with a semi-permanent glue usually made with a cyanoacrylate adhesive. Cyanoacrylate is found in commercial glues such as Super Glue® and Krazy Glue®. As one may guess, this would probably irritate the eye.
In addition to irritation, lash extensions can cause more serious problems for the wearer, including droopy eyelids and loss of natural lashes. More serious diagnoses include blepharitis, meibomian gland dysfunction, styes, and chalazia, all of which could lead to potential dry eye. Extensions can also cause allergic reactions and corneal scratches which could lead to scarring. Don’t know what these are? Continue reading!
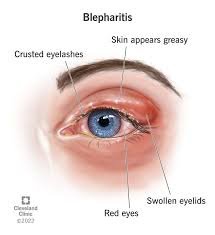
Blepharitis
Blepharitis is inflammation of the eyelids. Some of the signs of blepharitis include redness, swelling, soreness, and a burning sensation. Additionally, a crust can form at the base of the eyelashes. Blepharitis is caused by bacteria on skin or mites called Demodex. It is treated by keeping the eyelids and skin around the eyes clean using baby shampoo or over the counter eyelid wipes, and using warm compresses.
Meibomian Gland Dysfunction
Meibomian glands are oil glands located near the eyelashes, and play a significant role in tear production. Meibomian Gland Dysfunction, or MGD, occurs when these glands become clogged, causing eye irritation and inflammation. Some signs of MGD are dryness, burning, itching, redness, stickiness or crusting, watering, blurry vision, and foreign body sensation (the sensation that something is stuck in the eye). MGD can also lead to styes and chalazia. In the long term, inflamed meibomian glands may progressively die off, causing chronic dry eye. MGD is treated by using warm compresses, eye massages, eyelid scrubs, omega 3-fatty acids, and in severe cases, antibiotics.
Stye / Chalazion
Styes are red, painful lumps that can grow from the base of the eyelash, and are caused by an infection in the hair follicle. They usually present as a painful red bump with pus spots at the center of the bump. Symptoms include swollen eyelids, foreign body sensation, light sensitivity, excessive tearing, and crustiness along the eyelid margin.
A chalazion is a swollen bump on the eyelid caused by a clogged oil gland. They present as red and swollen bumps and can cause blurry vision. Both styes and chalazia often form as a result of severe blepharitis or meibomian gland dysfunction. They can be treated by using warm compresses for ten to fifteen minutes, several times per day at home. Additionally, an ophthalmologist may prescribe antibiotics or perform a steroid injection. Chalazia that do not resolve with conservative treatment can be drained via a small, outpatient procedure.
Allergies
Eye allergies are referred to as allergic conjunctivitis. The symptoms of allergic conjunctivitis include red, swollen, itchy eyelids and conjunctiva (the white part of the eye), burning or teary eyes, and light sensitivity. Unlike other types of conjunctivitis such as viral conjunctivitis (pink eye), this condition is not contagious. When the body’s immune system reacts to allergens in the eyes, it releases histamine along with other substances that cause the allergic reaction. Allergic conjunctivitis can be treated with preservative-free artificial tears, cool compresses, oral antihistamines, steroids, and anti-allergy eye drops.
An example of good extension hygiene
All in all, the risks of semi-permanent eyelash extensions may outweigh the cosmetic benefits. Other alternatives such as applying temporary eyelashes may not be as convenient, but are much better for your eye health. However, if you do have extensions or still want them, make sure to keep your lid and lashes clean with daily lid scrubs (face wash and water over the closed eyelids and lashes), and keep in mind that you are putting your eyes at risk for disease.